Hektoen & C.F. Perkins 1901
What is Sporotrix?
The genus Sporothrix belongs to the order Ophiostomatales, phylum Ascomycota, and includes thermo-dimorphic fungi known to change morphological form under temperature shifts, enabling them to switch from saprophytic to pathogenic form easily. This adaptation helped them spread in various habitats worldwide: soil, organic matter, like hay, crop plants, forest trees, moss, bark, and ambrosia beetles and mites.
Some Sporothrix spp. can be found on other fungi (Basidiomycota), and several are known as human and animal pathogens [1,2]. Infection caused by Sporothrix species is called sporotrichosis, infecting mainly cutaneous and subcutaneous tissues. Cats are important carriers of certain Sporothrix spores that can be easily transmitted to humans [3]. The genus was established in 1900 by Hektoen and Perkins after investigating and describing the species Sporothrix schenckii that caused infection of a wounded finger. Nowadays, the genus consists of 56 known species [4].
Sporotrix phylogeny
Sporotrix species have been inaccurately identified throughout the century since some generic diagnosis hadn’t been provided. Many Sporothrix species were classified under the genus Sporotrichum or Ophiostoma. Recent studies succeeded in separating economically and medically important species of the genus Sporothrix from Ophiostoma, but many Ophiostoma species were classified in Sporothrix and got new names. To fully resolve the Sporothrix genus and its phylogeny, a more extensive study needs to be done with a larger number of species, using several more conserved gene regions [4].
Which species does Sporotrix include?
Sporothrix currently includes 56 species that are widely distributed in various climatic zones and on completely different habitats. The first described and best-known species is S. schenckii, a name given after scientists Schenck, who first discovered the species but placed it in the Sporotrichum genus [4].
S. schenckii causes sporotrichosis and other species: S. brasiliensis, S. globosa, S. luriei, and S. mexicana. S. schenckii is mostly a human pathogen and could also be found in home dust [3,5,6]. At the same time, S. brasiliensis is an animal pathogen transmitted to humans after being scratched or bitten by an infected animal [3,5].
S. brasiliensis is the most virulent, S. schenckii is of intermediate virulence, while S. globosa is considered the less virulent one [7].
Probably, there are a lot of species of the genus Sporothrix that haven’t been discovered yet. Recently, 6 new species were described, originating from hardwood trees in Poland, named Sporothrix cavum, S. cracoviensis, S. cryptarchum, S. fraxini, S. resoviensis, and S. undulata [1].
Where can be Sporotrix found?
Sporothrix species are mainly present around temperate and tropical regions. It likes to grow in soil when the temperature is between 22°C (71.6°F) and 27°C (80.6°F), with pH between 3.5 and 9.4, and 90% humidity [2]. Species are thermo-dimorphic, meaning they can switch morphological form under the temperature shifts. When the temperature in the environment is around 22–25°C (71.6-77°F), species live as a saprophyte, growing with septate hyphae and forming conidia.
When inhaled into the lungs of humans or animals, where the temperature is around 37°C, it converts into its pathogenic yeast form [3,8]. Sporotrichosis can persist for many months in cats and can further spread by cat-to-cat or cat-to-human contact [3]. Sporotrichosis can also occur when wounded skin is in touch with the soil, plant, or organic material contaminated with Sporotrix [7].
How does Sporotrix look like?
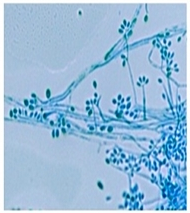
In the saprophytic asexual stage, species forms primary (sympodial) conidia that are thin-walled, hyaline, or slightly pigmented, obovoid or pear-shaped, 2-8×1.5-2.5 μm in size, positioned in a flowerlike arrangement at the end of the conidiophores (conidia-bearing structures) (Fig. 1).
Another form of conidia is called secondary (sessile) conidia which are thick-walled, dark brown, borne individually on short denticles, emerge from vegetative hyphae. Sessile conidia are 2-6 μm x 2-3.5 μm in size [9,10]. The sexual stage produces aseptate and reniform ascospores, carried in asci in dark brown to black ascocarps with large ostioles, with max size to 1 600 μm.
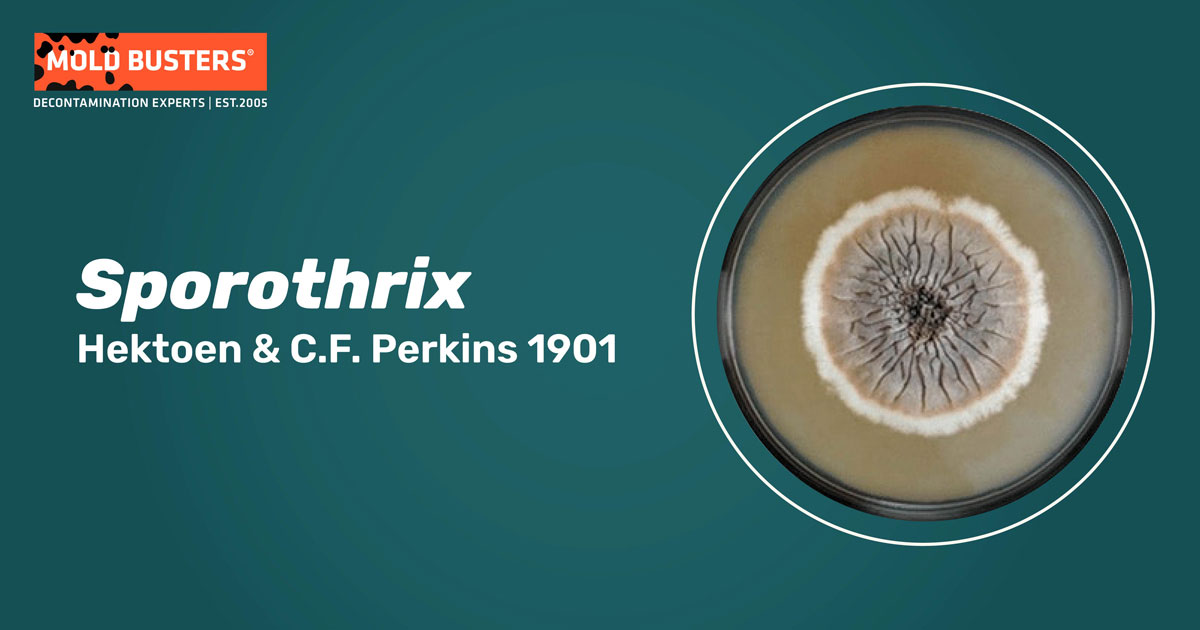
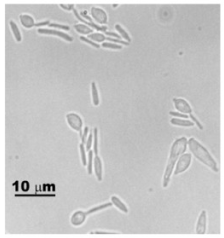
In the pathogenic phase, species convert into yeast, characterized by oval to spherical or elongated-cigar shape cells, 2–6 μm in size [10] (Fig. 2). Investigating similarity and differences in morphology of five Sporotrix species (S. brasiliensis, S. schenckii, S. globosa, S. mexicana, and S. albicans) it was found all species form pale orange to gray-orange colonies on PDA, with the diameter ranging from 15 to 38 mm after 21 days of incubation at 30°C (86°F).
All five species except S. globosa grew on 37°C (98.6°F), but none of them grew on 40°C (104°F). Differences are observed in sessile conidia shape. As S. brasiliensis and S. globosa form globose to subglobose conidia, S. mexicana forms similar but more ellipsoidal conidia, while S. schenckii forms completely different shape of conidia-triangular to cuneiform [9,10].
Is Sporotrix dangerous for humans?
A high incidence of sporotrichosis is found in Brazil, China, and South Africa [3]. It is among the most common mycoses (fungal infections) in urban areas, infecting mainly cutaneous and subcutaneous tissues that can spread to local lymphocutaneous tissue. Less frequently, it can spread on bones, joints, muscles, and the central nervous system [5,10].
Sometimes, pulmonary and systemic infections may occur [5], while sporotrichosis can progress into a severe infection in immunocompromised patients, resulting in high rates of hospitalization and even death [7]. In humans, the incubation period lasts from several days to three months, being most infectious between 1–3 weeks.
The severity and manifestation of sporotrichosis depend on pathogen virulence, amount, and type of inoculum (conidia or yeast), as well as the immune state of the host. The usual forms of sporotrichosis are cutaneous or lymphocutaneous infections of the extremities. Symptoms of cutaneous sporotrichosis begin with a localized lesion that becomes ulcerated, verrucous, or papular. Lymphocutaneous sporotrichosis overtakes the lymphatic system, and it is visible on the skin in the form of small nodules that become ulcerated and fistulised.
As cats are the most dominant vector of Sporotrix inoculums, an increase in cats population in the urban area (due to abandonment), neglecting cats health, or inadequate disposal of infected cat corpses, can lead to quick transmission of the disease, even epidemic [10].
Sporotrix infections are considerably higher in forestry workers and in people who handle wild and garden plant material in general. This is because Sporotrix spp. is commonly associated with certain forest mosses. During the 1990s, there were several incidences of Sporotrix infections in forestry workers handling pine seedlings, and the infecting pathogen was determined to be Sporotrix schenckii. Further investigation showed that most infections could be connected with workers handling pine seedlings found on a certain type of moss. The infection rate in workers who had handled evergreen seedlings and moss can be up to 17%. Therefore, it is always recommended to protect your hands when handling plant material, especially if it is unknown in origin [11, 12].
How to treat Sporotrichosis?
Since Sporotrix species are susceptible to antifungals, identification upon species-specific level is needed to choose appropriate treatment. S. brasiliensis is the most susceptible to antifungals both in vitro and in vivo, while S. schenckii, S. globosa, and S. mexicana happen to be less susceptible. If sporotrichosis is not treated properly, it can lead to severe problems [3]. Therapy depends on the severity of the disease and the patient’s immune status.
Effective compounds are considered to be potassium iodide and itraconazole, with promising effects of posaconazole, terbinafine, and amphotericin B. Different natural compounds showed promising effects like terpinen-4-ol, clotrimazole, coumarin derivatives, extracts of Piperaceae (pepper family), marjoram, and rosemary. Thermotherapy is successfully used in humans and cats, increasing skin temperature in the lesion area to 42–43°C (107.6-109.4°F) twice a day with a hot water bag [10].
Did you know?
The #1 toxic mold type found in kitchens in Canada is the Penicillium/Aspergillus mold group?! Find out more exciting mold stats and facts on our mold statistics page.
References
- Ostafińska A, Jankowiak R, Bilański P, Solheim H, Wingfield MJ (2021). Six new species of Sporothrix from hardwood trees in Poland. MycoKeys, 82: 1–32.
- Ramírez-Soto MC, Aguilar-Ancori EG, Tirado-Sánchez A, Bonifaz A (2018). Ecological Determinants of Sporotrichosis Etiological Agents. Journal of Fungi, 4(3):95.
- Rodrigues AM, de Hoog GS, de Camargo ZP (2015). Molecular Diagnosis of Pathogenic Sporothrix
- Species. PLOS Neglected Tropical Diseases, 9(12):e0004190.
- de Beer ZW, Duong TA, Wingfield MJ (2016). The divorce of Sporothrix and Ophiostoma: solution to a problematic relationship. Studies in Mycology, 83: 165–191.
- Rodrigues AM, de Hoog GS, de Camargo ZP (2013). Emergence of pathogenicity in the Sporothrix schenckii complex. Medical Mycology, 51:405–412.
- Marimon R, Gené J, Cano J, Trilles L, Dos Santos Lazéra M, Guarro J (2006). Molecular Phylogeny of Sporothrix schenckii. Journal of Clinical Microbiology, 44(9): 3251-3256.
- Silva-Bailao MG, de Sousa Lima P, Oliveira MME, Oliveira LC, Almeida-Paes R, Borges CL, Melo Bailao A, Guedes Coelho AS, de Almeida Soares CM, Zancope-Oliveira RM (2021). Comparative proteomics in the three major human pathogenic species of the genus Sporothrix. Microbes and Infection 23:104762.
- Gauthier GM (2017). Fungal Dimorphism and Virulence: Molecular Mechanisms for Temperature Adaptation, Immune Evasion, and In Vivo Survival. Mediators of Inflammation, Article ID 8491383.
- Marimon R, Cano J, Gené J, Sutton DA, Kawasaki M, Guarro J (2007). Sporothrix brasiliensis, S. globosa, and S. mexicana, Three New Sporothrix Species of Clinical Interest. Journal of Clinical Microbiology, 45 (10):3198-3206.
- Rodrigues AM, Portella Della Terra P, Gremiao ID, Pereira SA, Orofino-Costa R, de Camargo ZP (2020). The threat of emerging and re-emerging pathogenic Sporothrix species. Mycopathologia, 185:813–842.
- Powell, K. E., Taylor, A., Phillips, B. J., Blakey, D. L., Campbell, G. D., Kaufman, L., & Kaplan, W. (1978). Cutaneous sporotrichosis in forestry workers: epidemic due to contaminated sphagnum moss. JAMA, 240(3), 232-235.
- Coles, F. B., Schuchat, A., Hibbs, J. R., Kondracki, S. F., Salkin, I. F., Dixon, D. M., … & Morse, D. L. (1992). A multistate outbreak of sporotrichosis associated with sphagnum moss. American journal of epidemiology, 136(4), 475-487.
- Featured image photo, CDC/ Dr. Lucille K. Georg, assessed from phil.cdc.gov
Get Special Gift: Industry-Standard Mold Removal Guidelines
Download the industry-standard guidelines that Mold Busters use in their own mold removal services, including news, tips and special offers:

Written by:
Aleksandra Zebeljan
Mycologist
Mold Busters
Edited by:
Dusan Sadikovic
Mycologist – MSc, PhD
Mold Busters
